

- #ALLWELL MEDICARE TIMELY FILING LIMIT HOW TO#
- #ALLWELL MEDICARE TIMELY FILING LIMIT CODE#
- #ALLWELL MEDICARE TIMELY FILING LIMIT FREE#
#ALLWELL MEDICARE TIMELY FILING LIMIT FREE#
In case, you’re looking for some additional information, feel free to contact us or comment below.Clean claim resubmissions must be received no later than 12 months from the date of services or 12 months after the date of eligibility posting, whichever is later. In this article, I have mentioned everything you need to know about timely filing limit along with the timely filing limit of all major insurances in United States. Also ask your accounts receivable team to follow up on claims within 15 days of claim submission. If insurance company allows electronic submission then submit claims electronically and keep an eye on rejections. DEPARTMENT OF HEALTH AND HUMAN SERVICES OFFICE OF INSPECTOR GENERAL.

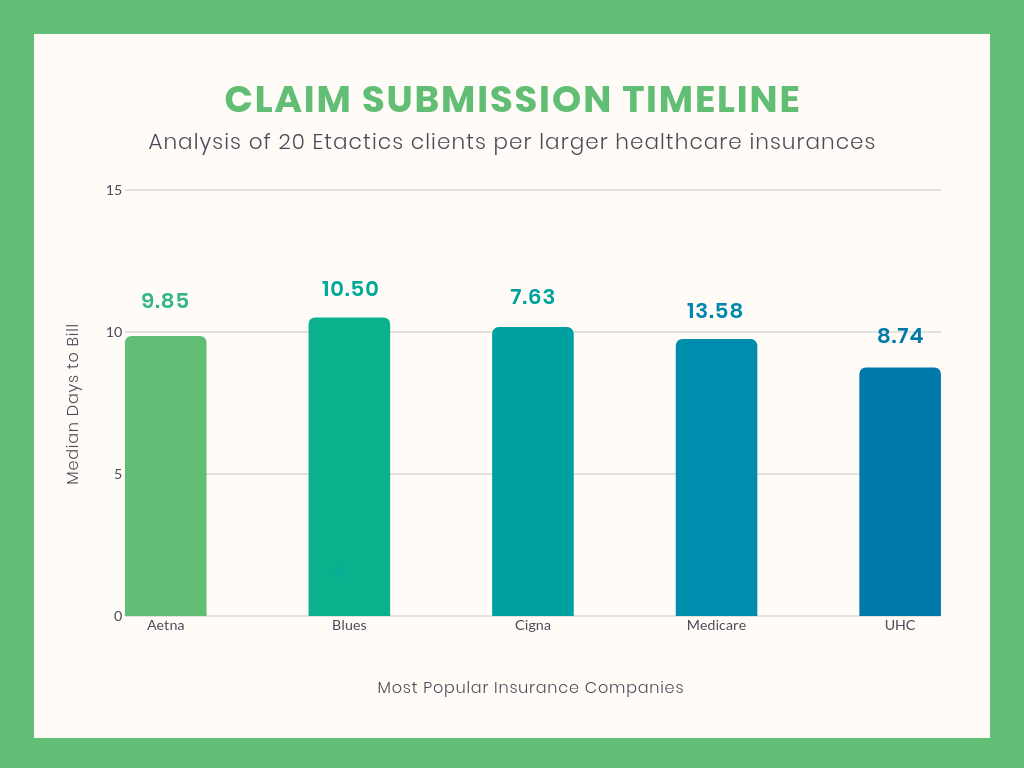
Below, I have shared the timely filing limit of all the major insurance Companies in United States. However, Medicare timely filing limit is 365 days. Your patients have a choice in their Medicare health insurance. The timely filing limit varies by insurance company and typically ranges from 90 to 180 days. A claim must be filed on the proper form, such as CMS 1500 or UB 04. MEDICARE MEMBERS: PROTECT YOURSELF AGAINST MEDICARE FRAUD AND IDENTIFY THEFT THE U.S. The Annual Enrollment Period for your Medicare patients runs from October 15 to December 7, 2021. Others have been described throughout the body of this manual. Allwell Medicare (HMO) Allwell Medicare Select (HMO) Allwell Medicare Premier (HMO). Some of these requirements are found in your Participation Agreement. A claim is a request for reimbursement either electronically or by paper for any medical service. MEDICARE REGULATORY REQUIREMENTS As a Medicare contracted provider, you are required to follow a number of Medicare regulations and CMS requirements. Encounters do not generate an Explanation of Payment (EOP). To avoid timely filing limit denial, submit claims within the timely filing limit of insurance company. DHS and by the Centers for Medicare and Medicaid Services (CMS). requirements, the rejected claim should be resubmitted within timely filing limits based on the date of service (those limits are described above under.
#ALLWELL MEDICARE TIMELY FILING LIMIT HOW TO#
How to avoid from claim timely filing limit exhausted? What if claim isn’t sent within the timely filing limit?įailing to submit a claim within the timely filing limit may result in the claim being denied with a denial code CO 29, so it is important to be aware of the deadline and submit the claim promptly. No reimbursement will be made for claims received beyond this date.

Unitedhealthcare Non Participating Providers The Medicare timely filing requirement is one calendar year from the date of service this includes resubmission of corrected claims that were not able to be processed. Medicare flex cards are offered by specific Medicare Advantage plans. Keystone First Resubmissions & Corrected Claimsġ80 Calender days from Primary EOB processing dateġ2 months from original claim determination ) Need to telephone us on behalf of someone else. Amerigroup for Non Participating Providers


 0 kommentar(er)
0 kommentar(er)
